Newsletter
The College of Reproductive Biology (CRB) is a not-for-profit special interest group of the American Association of Bioanalysts (AAB).

A Great Grey Rhino in the Room: The Human Capital Conundrum in ART
Carol Lynn Curchoe, Ph.D., HCLD(ABB)
In the USA, The IVF industry is experiencing a pressing, double-edged problem: it struggles to fill new embryologist positions, an estimated 5% of the existing workforce is already beyond retirement age (65-67 years old)—and an estimated additional 20-40% will reach retirement age within the next 7 years. Embryologists are the core of the IVF supply chain, and a shocking grey rhino (an obvious yet ignored threat) is in the room. We cannot make more embryos without more embryologists. By all predictions, the IVF industry is on track to grow astoundingly in the next ten years as millennials who have put off childbearing for career begin to seek age-related infertility care. We are so focused on growing good embryos, but how do we grow (attract) new embryologists?
An ASRM practice document “Minimum standards for practices offering assisted reproductive technologies: a committee opinion” states that:
“There should be a contingency plan in place for all personnel essential to a program in case of illness, absence, or departure of an individual from the program. The purpose of the contingency plan is to ensure that critical operations within the laboratory and practice are covered without interruption.”
Our entire field is in dire need of a contingency plan.
40% of our current workforce is attributed to the “Baby Boomer” generation. The oldest Baby Boomers are 75 years old, and the youngest are now 58. I would wager to guess that the vast majority of 67-75 year olds have already retired. Just think of the IVF lab directors and embryologists you know who will retire in the next 5-7 years (i.e., the 58-65 year olds). Each one likely directs numerous offsite laboratories. And new IVF laboratories open every day. Are enough new HCLD certificates being granted to ensure that IVF labs can continue to function at high levels of patient care and quality after this looming tsunami of retirements?
As a result of this human capital conundrum, it has become even more important that IVF clinics ensure knowledge transfer, retention, and upskilling occur.
Knowledge Transfer
In “The in vitro fertilization laboratory: teamwork and teaming” the authors note that “Knowledge sharing is vital among an IVF laboratory team to build on the knowledge base and enable succession and development. Clinical case review, journal-based learning, and research opportunities all facilitate such sharing and knowledge building.” Embryologists who are struggling to simply complete the expected clinical laboratory work of the day may not be able to fulfill these ideals, as well as train and supervise junior team members.
The model of meeting for scientific congresses, where this type of knowledge transfer typically occurs, was briefly derailed during the global coronavirus pandemic. Scientific congresses can only serve a fraction of embryologists. The long overdue International IVF Initiative (I3) rose, modernizing the age-old practice of knowledge transfer with the added benefit of democratizing access for embryologists worldwide. Alternate approaches to further modernize the concept of “knowledge transfer” in embryology and the ARTs are so important. Chocair et al proposed a robust roadmap to modernize knowledge transfer that includes multiple digital methods; online self-assessment programs, digital technology integration through blogs, podcasts, and influential videos, an online platform education management platform to report training logbooks, including a “knowledge assessment passport” among other action items. The Y and Z generations of workers are digital natives (digital “junkies” even...) they cannot live without their mobile devices. Investment in and support for “digital first” knowledge transfer technologies is essential. (Full disclosure, I am the inventor of one such unsupported technology, the ART Compass mobile app, so it goes without saying, these opinions are biased).
Embryologist Retention
There is a childcare crisis in the USA. The majority of embryologists are women of childbearing years. These two things are essentially incompatible.
Embryologist schedules are unpredictable (consider the odd 100 egg retrieval or 6-hour TESE) and can start well before a school day begins and stretch until well after a school day ends. Additional childcare considerations must be made for holidays and weekend shifts. That doesn’t even take into consideration the mental anguish of missing significant family related events or milestones. An added consideration is that families rarely reside in multi-generational households (or even in the same city) and Baby Boomers are no longer retiring in a timely fashion due to a combination of economic fragility brought on by multiple successive economic failures and longer life-spans. Even when they do retire, they don’t necessarily want to watch little ones. They have already raised their own children and are ready for travel, adventure, and leisure. Many embryologists are confronted with a very simple calculus: “Do I make enough in one hour to cover one hour of childcare?” With the skyrocketing cost of childcare as well as the scarcity of available childcare providers, too often that answer is “no.”
One action item for the field at large is to train more male embryologists. Diversifying the workforce will have numerous benefits; including, greater insulation from multiple maternity leaves of absence. However, an even more pressing need is to fix the culture of IVF practices to be less rigid, less demanding, and more flexible for those with families or even without, recognizing that work life balance will drive the decisions of Gen Z and Gen Y. And to do that, we must support the elevation of our female embryologists to the highest ranks (PhD/HCLD). It stands to reason that if 80% of embryologists are female, 80% of lab directors should also be female. However, we see the opposite is true. It is clear that when men do become embryologists, they quickly ascend the ranks to become lab directors, or presumptuously, I think they must leave the field because they won’t stand for the intense hours/low pay/holidays and weekends. So modulating the intense, unpredictable “culture” of IVF labs should have the impact of retaining both genders equally.
Upskilling
In the USA, we have few formal "embryologist" education, training, or placement programs. The bulk of all new embryologist training falls to the senior embryologists. This dearth, coupled with high embryologist demand has led to the rise of a number of commercialized and privatized training programs to fill the void. Currently, these programs have stellar reputations. But what is to stop predatory programs from also springing up? Generally, consumers of education programs have some level of assurance and transparency because there is oversite and regulation of higher education. Results are measurable and formally assessed and documented, sources of capital and cash flow are understood, the quality of training and/or placement is guaranteed. One action item for the field could be a standardized and digital education management platform to report training logbooks, that includes the “knowledge assessment passport” mentioned above. One example, and in response to the COVID-19 pandemic, the American Center for Reproductive Medicine (ACRM) transitioned its annual training to a fully online modules included manual semen analysis, sperm morphology and ancillary semen tests (testing for leukocytospermia, sperm vitality, and anti-sperm antibody screening).
Conclusion
Within higher education, abundant models exist for hands on biotech training at the “associate degree” open enrollment level, but grow scarcer at the BS / BA level. Advocacy associations for the ART industry might focus lobbying efforts at State legislature levels that acknowledge that without an appropriately skilled workforce, it is impossible to grow this highly-regulated industry. Local ART education programs should eliminate barriers to ART careers by providing access to expensive equipment, space, and real-life education through hands-on learning opportunities, learning FDA, CLIA and other regulatory requirements that result in highly employable, and valuable technical careers in ART. A groundbreaking new study, Clinical Laboratory Workforce: Understanding the Challenges to Meeting Current and Future Needs suggests further innovative ways to improve workforce recruitment and retention, including; financial incentives to encourage professional development and job satisfaction; and flexible schedules, benefits, tuition incentives, and sign-on bonuses.
REFERENCE
- Palmer GA, Tully B, Angle M, Sadruddin S, Howles C, Nagy ZP, et al. Occupational Demand & Resultant Stress of reproductive scientists: Outcomes from an International survey. Unpublished Online survey by the educational platform International IVF Initiative.
CRB News Articles
06/15/2022
Vol 11, No. 1
06/15/2022
Announcing the CRB Andrew Runge Memorial Embryology Scientist Research Grant Award
06/15/2022
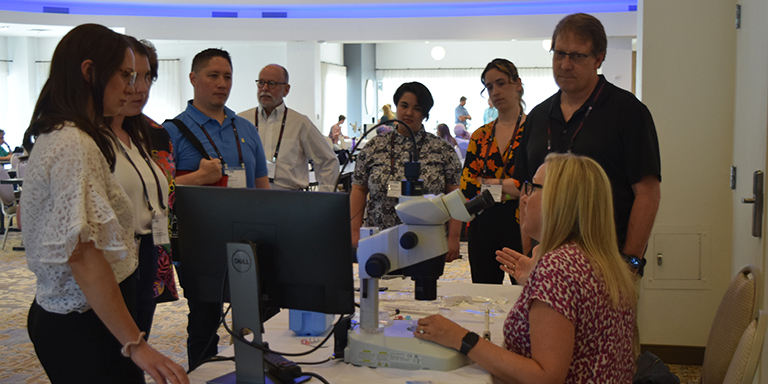
CRB 2022 Symposium Recap
06/15/2022
From the President
06/15/2022
ALS/ELS Certifications for Andrologists and Embryologists
06/15/2022
Publication Committee
06/15/2022
Under Pressure: A Survey on Stress and Clinical Embryology
06/15/2022
Earn ABB/PEER Continuing Education Credit Attending Postgraduate Courses at ASRM 2022
06/15/2022
A Great Grey Rhino in the Room: The Human Capital Conundrum in ART
CRB Standing Rules - Log in to view