
Newsletter
Special Interest Group of the American Association of Bioanalysts (AAB)
IVF in the Time of Corona
Marina Gvakharia, M.D., Ph.D, HCLD/ELD(ABB)
Palo Alto Medical Foundation, Sutter Health, San Jose, California
My father used to refer to me as “the one with a scary job." And this was way before COVID-19 pandemic. I often wonder what he would think about me running a busy IVF laboratory during a deadly global pandemic while trying to stay alive, keep my team safe and healthy, and do right by the patients. I am sure many of you, my fellow scary-job-holders, can relate. I am also sure everyone has a story about how they coped. We are all ARTists after all: resourceful, creative, smart, and fearless. We always find a way.
My team and I feel that as we were working together and brainstorming our COVID-19 protocols, this crisis brought us closer together and made us stronger in many ways. This is our COVID story.
Part One: The Shutdown
On March 8th, as the COVID-19 crisis was unfolding, we mandated masks, social separation and enhanced cleaning procedures. We also identified a “dedicated survivor," who was isolated and working from home on standby to step in if the team gets infected. However, with each passing day, it was becoming painfully obvious that these measures were not going to be enough. Cases were climbing, shelter-in-place rumors were circulating, and public health officials were calling to tally-up anesthesia machines and beds in our surgery centers in case hospitals became overwhelmed. Staff were scared. By mid-March, our practice decided to completely shut down cycles in order to help with the shelter-in-place efforts and protect our patients and staff while we figured out optimal ways to re-open safely. ASRM recommendations to stop cycling non-emergent cycles came out shortly after, and we were in full support of this document.
We stayed closed for over 8 weeks. During this time, we had only one team member on site in order to take care of our cryotanks and accept gas deliveries. For this person, we essentially created “shelter in place” conditions – no visitors, no contact with clinical team, minimal time on site. Everyone else worked from home on various projects and educational activities. For instance, we took advantage of the ASRM offer to enroll in embryology and andrology certificate courses and had study sessions together. We tackled a number of projects that were waiting for “when we have time." Now, sadly and unexpectedly, we had the time. But most importantly, we worked hard on designing our new COVID-19 policies and procedures for when we finally could go back to work.
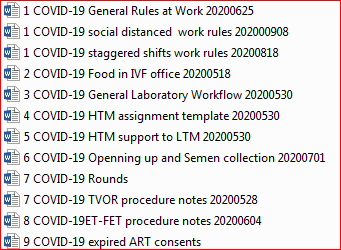
I often consult with Dr. Atul Gawande’s writings for my management decisions. (Side note: If you have not read The Checklist Manifesto, drop everything and do it now. You are welcome.) He didn’t disappoint this time either. He never does. His May 13, 2020, piece in the New Yorker, "Amid the Coronavirus Crisis, a Regimen for Reentry," is a very useful review of the successful processes at Mass General Hospital, as they were able to protect their staff and patients during the surge, while caring for extremely sick and infectious COVID patients. Here is the link to this great resource: https://www.newyorker.com/science/medical-dispatch/amid-the-coronavirus-crisis-a-regimen-for-reentry. All we had to do is extrapolate their experience to our reality. And extrapolate we did. This is just a partial snapshot of our COVID SOP folder.
Fortified with a good plan, we felt we now were ready to return to work and do our magic in a safe environment.
Part Two: Partial Opening
In June, armed with our new protocols and with the ASRM blessing, we started cycling patients at approximately 50% capacity.
Presented below are several areas that we’ve identified for our targeted intervention:
- Daily screening
- Self-screening with special attention to mild symptoms before coming to work.
- At the door daily screening of all employees, patients, and visitors for symptoms of COVID-19.
- Promote culture where coming to work sick is not considered heroic.
- Staff is provided with coaching about staying safe outside work and other COVID-19 resources.
- Masks
- Surgical masks are worn by everyone at all times.
- N95 masks are worn when physical distancing is not possible.
- Physical (social) distancing
- Lab staff were separated into two never-overlapping teams. At first, we worked weekly shifts with one team on site and the second team providing clerical support from home. Clerical support included answering emails, responding to phone calls, charting into EMR, and remote second ID checks for procedures via FaceTime. Once we became busier, it became harder for one on-site team to handle all laboratory procedures for the entire week. So we switched to staggered shifts: first team would work until 12-1 pm with home clerical support by the second team. First team would disinfect the lab at the end of their shift and switch to home support for the second team, who would come in at 1:30 pm and work until procedures were finished.
- We observe strict distancing rules within the laboratory where only 3 people are allowed at any given time.
- We completely eliminated patient contact and now use phone, email, and EMR to communicate with patients.
- Minimized/eliminated face-to-face contact with MDs, nursing and other staff and used email, Slack, FaceTime, and other platforms instead.
- Closed access to embryology suite for all except laboratory staff and gas deliveries.
- All embryologists’ clerical functions were done from home offices.
- On-site clerical staff protected from non-essential contact with laboratory and other staff.
- We developed special SOPs for touchless semen acceptance.
- We minimized semen collection room use – only one on-site collection per day is allowed.
- Hygiene
- Proper hand-washing (20 seconds, proper technique)
- Disinfecting surfaces, especially common and high touch areas.
- No tool-sharing (individual “toolboxes” for “strippers," pipettes, timers, calculators, pens, etc. for each team member.)
Kausi Sellakkannu made this awesome video about our COVID-19 life, which we are including here for your viewing pleasure.
Part Three: Full Opening
Surprisingly, we soon learned that demand for our treatments has increased after the COVID shutdown. This seems to be the trend around the country, which is interesting and probably warrants a closer look to examine the reasons why patients are eager to become pregnant during this global pandemic. But this topic is for another day.
After approximately two months of reduced capacity, we gradually increased our caseload in order to meet patients’ needs. With increased demand, we realized that staggered shifts were not giving us the necessary manpower during the day. It just seemed as if each team was short one person at all times. As COVID cases started slowly decreasing in our area, we made the decision to relax our “no overlap” rules and now allow as many staff on site as needed while still observing physical distancing, masking, hand-washing, and other rules. Staff are encouraged to leave once their bench work is done and work from home for the rest of the day.
Currently, with the exception of the team separation rule, we still follow all the guidelines listed above. We are essentially sheltering in place at work in our little bubble with not much contact with the outside world. It certainly is isolating. At times these procedures seem as if they are a tad too much, and sometimes we feel an urge to relax some of them. But then I remind myself of several of our clinical staff who tested positive and of an infectious patient spending a couple of hours on the premises. So we continue with keeping calm and sheltering in place. Thankfully, our system has kept our laboratory team safe so far and we are grateful. Hope you and yours are safe too!
Special thanks to Sue Lee, Kausi Sellakkannu, Sandra Ortiz, Sarah Chacon, Yining Li, Angie Sawyer, and Julie Gomez for their support of our joint mission of keeping our work family protected, healthy, and safe.
P.S. This piece was written before this current third wave of COVID, when things were looking up a bit. Of course now we have more reasons to be worried. California is under stay-at-home orders and another shutdown of non-emergent medical services may not be out of question. Naturally, we worry about potential lockdown, but at least now we have a functional playbook in case we have to go through these steps again. Let’s hope it will not come to that, but now it is not the time for complacency. Stay vigilant and stay safe. Godspeed!
Comprehensive Training for your IVF Lab ⇒CRB News Articles
12/10/2020
Vol 9, No. 3
12/10/2020
From the President and Committee Chairs
12/10/2020
IVF in the Time of Corona
12/10/2020
Comprehensive Training for your IVF Lab
12/10/2020
Embryology 3.0: ARTs of the Future will be Guided by Artificial Intelligence Systems
12/10/2020
AAB Free Recorded Webinars
12/10/2020
25th Annual CRB Symposium
12/10/2020
CRB Free Recorded Webinars
CRB Standing Rules - Log in to view



