Newsletter
Special Interest Group of the American Association of Bioanalysts (AAB)
Witnessing in ART – Has the time come to utilize technology?
Carli W Chapman, ELD/TS(ABB), Reproductive Medicine Institute, Oak Brook, IL
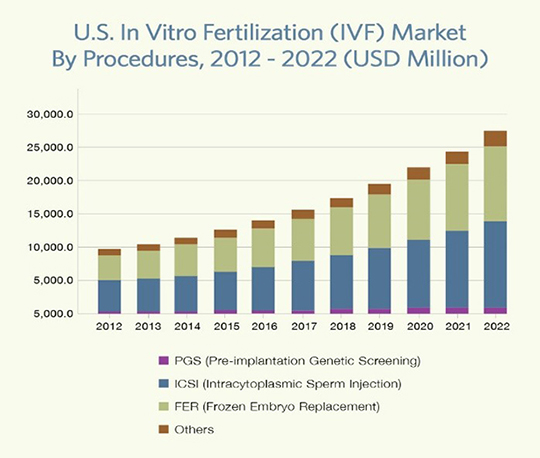
Assisted reproductive technologies (ART) has become a maturing global industry. In the US use of ART has continued to increase each year. With this increase comes increasing clinic revenues and patient load. Has the time come to invest in witnessing technologies for clinics?
There are multiple steps in ART procedures where gametes and/or embryos could potentially be mixed up. This is a DEVASTATING prospect for the potential parents involved, as well as the clinic. The emotional impact of such a mistake does not only affect the gamete donors involved, but all clinic staff and laboratory personnel, whether directly involved or not. Additionally, the legal and financial burden of such a mistake can lead to clinic closings.
IVF clinics in the US routinely use “double witnessing” in which one person witnesses the actions of another person. This procedure was adopted from the medical industry’s independent double checks. This procedure is also fraught with dangers, especially in a busy clinic with multiple procedures going on daily. Many IVF clinics in the US may only have one person working in the IVF lab on any given day. Who is providing “witness” for them?
The problems with the most common system of using another person to provide independent double check include:
- The witness may not be properly trained in the “Witnessing Procedure” particularly for embryologists working alone calling in a phlebotomist, receptionist or nurse to verify.
- The witness may be interrupted from their immediate task and provides only cursory witness not an independent cognitive task.
- Who is the responsible person? The person providing the independent witness or the person completing the task asking for verification?
- Data from the nursing industry indicates that double witnessing does provide sufficient verification.
- Double checks depend of one fallible person assessing another fallible person’s work.
- Most laboratories do not have a detailed witnessing procedure. The procedures routinely say something to the effect of “. . . .verified by …..(another person). The details of how this witnessing occurs are rarely delineated. Who provides witnesses? How is that person trained in the witnessing process? How is that person summoned to witness? How is the witness documented? Does the procedure specifically say, “interrupt someone”? Who is the responsible person? The witness or the person completed the task? Does the procedure explicitly say what needs to be checked and how it is checked? Do I hold up a labeled tube of sperm and say this is John Doe and I am inseminating Jane Doe?
The Human Fertilization and Embryology Authority of the UK states “electronic systems such as barcoding and radio frequency identification (RFID) for assisted conception are appropriate.’ The tasks in the process ‘do not need to be manually witnessed if an electronic system is being used.”
There are multiple electronic witnessing systems on the market. RI Witness (RFID technology and Matcher (Barcode Technology) are the most widely used. There are numerous others newly on the market or coming to the US market such as Gidget, Fertiproff, eIVF Biometrics. All of the systems on the market can reduce the risk of IVF misidentification, provide traceability of who, what, where, when, replace manual processing, eliminate the need for handwriting on dishes, provide real time quality data, improve compliance and add to cost savings by eliminating the “witness”. These systems integrate with your existing IT systems and EMRs.
This is a technology whose time has come. The ease of use and effective documentation of gamete handling should not be cost prohibitive to our industry. The time electronically witnessing an IVF cycle is ½ the amount required with manual witnessing. The confidence these devices provide staff cannot be overstated. Patients feel more secure knowing there is a non-human witnessing system in place monitoring their gametes in the laboratory and during transfer process.
Carli Chapman, ELD/TS(ABB)
Forte, M. et al. Electronic Witness System in IVF – Patients perspective. JARG 2016 339(): 1215.
Grant, D. Navigating Independent Double Checks for Safer Care: A Nursing Perspective. University of New Hampshire Scholars; Repository Honors Thesis.
Thornhill et al. Reducing human error in IVF with electronic witnessing. F & S 2011 96(3) Supplement P245.
Rienzi et al. Failure mode and effects analysis of witnessing protocols for ensuring traceability during IVF. RBM Online 2015
CRB News Articles
10/1/2019
Vol 8, No. 2
10/01/2019
From the President
10/01/2019
Credentialing and Membership Committee
10/01/2019
Legislative Committee
10/01/2019
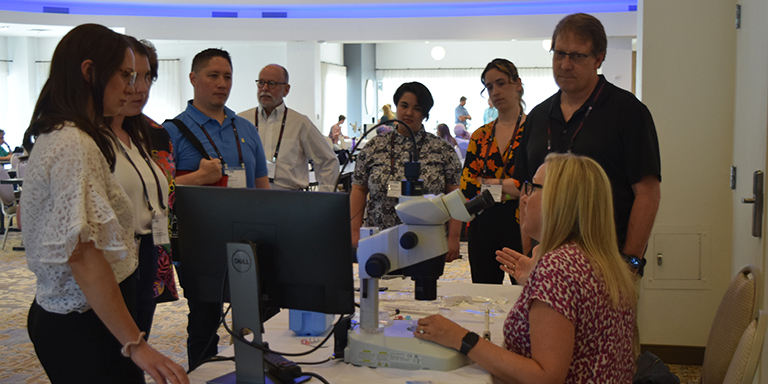
Meeting Committee
10/01/2019
Publications Committee
10/01/2019
Standing Rules Committee
10/01/2019
Witnessing in ART - Has the time come to utilize technology?
Save The Date:
2020 CRB Symposium – May 7-9, Orlando
CRB Standing Rules - Log in to view